Дефект межпредсердной перегородки
Что такое Дефект межпредсердной перегородки?
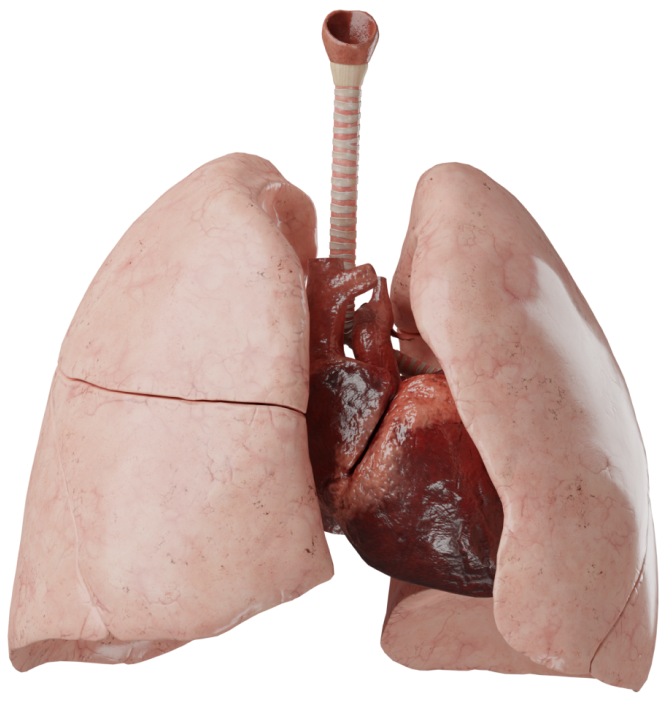
Дефект межпредсердной перегородки - врожденный порок сердца, характерной особенностью которого является наличие отверстия в межпредсердной перегородке. Может быть как самостоятельным пороком сердца, так и составной частью других пороков.
Эмбриология
Развитие вторичного ДМПП связано с нарушением перехода от эмбрионального к взрослому кровообращению. В норме первичная перегородка закрывается после рождения, из-за повышения давления в левом предсердии. В случае отсутствия первичной перегородки и происходит развитие вторичного ДМПП. Первичный дефект - развивается вследствие нарушения формирования эндокардиальных подушек. Дефект в области коронарного синуса связан с неправильным формированием общей стенки между коронарным синусом и левым предсердием. Дефект по типу sinus venosus часто сочетается с аномальным дренажем легочных вен.
Его развитие происходит в результате нарушения процесса формирования системных и легочных вен.
Анатомия
Первичный ДМПП располагается непосредственно над атриовентрикулярными клапанами, и его нижним краем является перегородка между клапанами; крайним вариантом патологии является общее предсердие. В изолированном виде встречается чрезвычайно редко, чаще сочетается с общим атриовентрикулярным каналом и другими аномалиями сердца.
Вторичный ДМПП характеризуется обязательным наличием края межпредсердной перегородки между дефектом и атриовентрикулярными клапанами. Дефекты могут быть множественными, различными по размеру и расположению.
Дефект венозного синуса также редкая патология, располагается он обычно около места впадения верхней полой вены, в редких случаях - в месте впадения нижней полой вены. Часто сочетается с аномалиями впадения легочных вен или является составной частью синдрома ятагана.
Дефект в области коронарного синуса обнаруживается в той части межпредсердной перегородки, куда открывается отверстие коронарного синуса. Таким образом, левое предсердие оказывается связанным с правым через венозный коронарный синус.
Классификация
- Первичный;
- Вторичный;
- По типу sinus venosus;
- В области коронарного синуса.
Гемодинамика
Основой нарушений кровообращения является сброс крови через дефект из одного предсердия в другое. Направление и величина шунта определяются градиентом давления между предсердиями, в меньшей степени размером и локализацией дефекта.
Обычно давление в левом предсердии выше, чем в правом, что определяет лево-правый сброс крови, приводящий к диастолической перегрузке правого желудочка и гиперволемии малого круга кровообращения. По мере развития ребенка происходит снижение общелегочного сопротивления, увеличивается податливость правого желудочка. В это же время возрастают ОПСС и ригидность левого желудочка. Результатом данных изменений является нарастание сброса крови через ДМПП слева направо, и это направление остается доминирующим в последующие годы.
Локализация отверстия возле устья полой вены может сопровождаться сбросом венозной крови в левое предсердие даже при равенстве давления в предсердиях.
Значительная резервная емкость, низкое сопротивление легочных сосудов и перегрузка малого круга кровообращения объемом, а не давлением, позволяет избегать развития легочной гипертензии. Легочная гипертензия развивается, как правило, спустя длительное время и только у лиц с наследственной предрасположенностью.
Таким образом, основными последствиями ДМПП являются объемные перегрузки правого предсердия и желудочка, а также гиперволемия малого круга кровообращения.
Правый желудочек длительное время в состоянии компенсировать возникшие гемодинамические проблемы, что сопровождается увеличением функциональной нагрузки, постепенным развитием гипертрофии и ухудшением растяжимости. Также, дилатация правого предсердия приводит к развитию недостаточности трикуспидального клапана и нарушениям ритма.
Диагностика
- Допплер-ЭхоКГ. Визуализация дефекта: размер, местоположение, количество дефектов и т. д.
- Рентген органов грудной клетки. Увеличенная тень сердца, правый желудочек или правое предсердие, увеличенный сосудистый рисунок легких, легочная артерия расширена. Пациенты с небольшими дефектами часто не имеют изменений.
- ЭКГ. Изменения на ЭКГ неспецифичны. Возможно обнаружить отклонение ЭОС вправо, неполная блокада правой ножки пучка Гиса.
- КТ, МРТ. Полезно в случаях сложной анатомии дефекта, когда он сопровождается другими ВПС.
- Катетеризация полостей сердца. Проводится пациентам с высоким давлением в системе легочной артерии по данным ЭхоКГ для определения легочного сосудистого сопротивления, а также для уточнения наличия сопутствующих патологий.
Клинические проявления
Клинические проявления зависят от размера, расположения дефекта и сопутствующих аномалий. При больших дефектах симптомы сердечной недостаточности могут развиваться в раннем периоде. Небольшие дефекты могут не проявлять себя клинически много лет, из-за длительной гемодинамической компенсации. В раннем возрасте единственным проявлением может быть транзиторный цианоз - смена шунта на право-левый при плаче, беспокойстве. Как правило, нарушения физического и психического развития детей не происходит.
При больших дефектах уже в раннем периоде могут развиваться симптомы сердечной недостаточности: бледность кожных покровов, тахикардия, отставание в физическом развитии, нарушения при кормлении и т.д. Для таких детей характерно наличие рецидивирующих легочных инфекций из-за гиперволемии малого круга кровообращения. У детей более старшего возраста с небольшими по размеру дефектами могут наблюдаться обмороки, быстрая утомляемость, одышка при физической нагрузке.
Лечение
Хирургическое лечение обычно проводят в возрасте 2 лет, при отсутствии показаний к лечению в более раннем возрасте. Наличие дефекта размером более 5 мм или соотношение Qp/Qs более 1,5:1 - показание к операции, по мнению некоторых авторов. Небольшие дефекты склонны к спонтанному закрытию в первые два года жизни. Закрытие дефекта межпредсердной перегородки возможно открытым и эндоваскулярным методом. Эндоваскулярное закрытие применяется для вторичных дефектов. Для этого метода существуют ограничения, связанные с размером и формой ДМПП.
Для эндоваскулярных операций применяется окклюдер, который проводится через бедренную вену и раскрывается в области межпредсердной перегородки, закрывая ее. Открытые вмешательства подразумевают ушивание (при небольших дефектах) или закрытие с помощью заплат, чаще из аутоперикарда.