Обструкции выводного отдела левого желудочка
Что такое Синдром обструкции выводного отдела левого желудочка?
Синдром обструкции выводного отдела левого желудочка может возникнуть вследствие клапанного, субаортального и надклапанного стеноза.
Эмбриология
На 4-й неделе формирования зародыша общий артериальный ствол разделяется на два магистральных сосуда (аорту и легочную артерию) путем образования внутренней перегородки за счет инвагинации эндокарда по двум бороздкам. Разделение возникает между IV и VI аортальными дугами и продолжается вниз. Продолжением аортального канала являются сосуды, происходящие из IV аортальных дуг (из них образуется окончательная дуга аорты и плечеголовной ствол), а продолжением легочного канала — сосуды, происходящие из VI аортальных дуг (из них образуются открытый артериальный проток и часть правой легочной артерии).
Правый желудочек соединяется с VI аортальными дугами (легочные артерии), а левый — с III и IV дугами. На более позднем этапе развития зародыша со стороны внутренней стенки устьев сформированных магистральных сосудов образуются утолщения, состоящие из мезенхимальных подушечек, из которых формируются четыре створки артериальных клапанов. После разделения луковицы на два выводных тракта одна пара створок дополнительно делится на две части. В результате образуется шесть клапанных створок, из которых три створки образуют клапан легочной артерии, а другие три — клапан аорты. Одновременно с этим формируются AV-клапаны за счет утолщения мезенхимы (так называемые эндокардиальные подушечки).
В многочисленных исследованиях показана семейная предрасположенность к порокам аортального клапана.
Нарушения кардиогенеза на стадии формирования выводного отдела левого желудочка могут привести к возникновению данной группы пороков.
Классификация
- Клапанный аортальный стеноз;
- Субаортальный стеноз;
- Дискретная субаортальная мембрана;
- Туннельная форма субаортального стеноза;
- Гипертрофическая кардиомиопатия;
- Структурный субаортальный стеноз;
- Надклапанный аортальный стеноз.
Клапанный аортальный стеноз
Анатомия
Аортальный клапан может быть двух или трехстворчатым. Створки клапана сращены по комиссурам, с небольшим отверстием в центре. Также створки часто утолщены, малоподвижны.
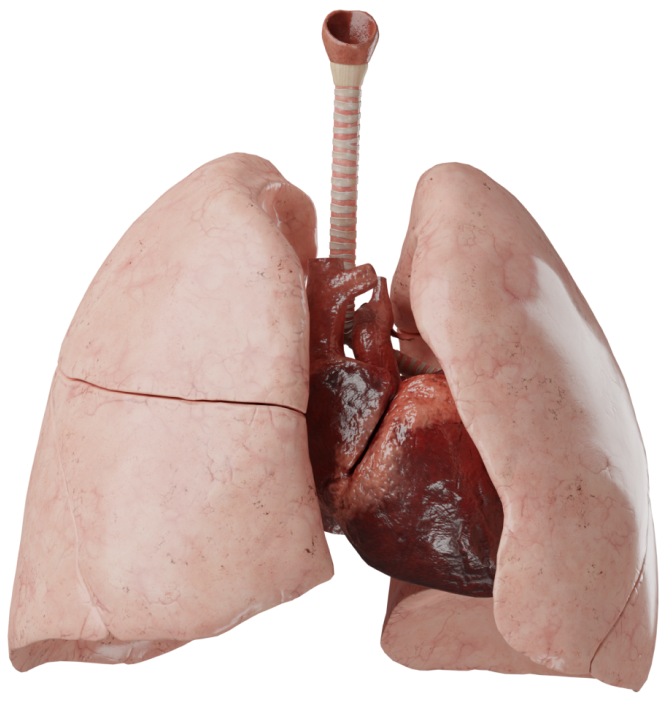
Гемодинамика
Сужение клапана создает градиент давления между левым желудочком и аортой во время систолы. Поскольку кровоток через суженный клапан имеет турбулентный характер, градиент не является простой линейной функцией потока.
Он прямо пропорционален площади сечения клапана, поэтому удвоение объема кровотока через клапан увеличивает градиент в 4 раза. Величина градиента зависит от сократимости левого желудочка и сопротивления периферических сосудов.
Для оценки гемодинамической тяжести обструкции необходимо измерить объем кровотока через клапан и одновременно градиент.
Среднее давление в левом предсердии обычно нормальное, если нет тяжелого сужения. У большинства детей со стенозом аорты конечно-диастолическое давление в левом желудочке находится на уровне верхней границы нормы. Его повышение указывает на ухудшение функции левого желудочка или на выраженную гипертрофию и снижение комплаенса этой камеры.
Кровоснабжение миокарда снижено, несмотря на проходимость коронарных артерий.
Диагностика
- ЭхоКГ, КТ, МРТ. Визуализация дефекта.
- Рентгенография ОГК. Можно обнаружить расширение тени аорты. Резко выраженная талия сердца.
- ЭКГ. Характерные изменения отсутствуют или имеются признаки гипертрофии левого желудочка.
- Катетеризация сердца и ангиокардиография. Применяется для уточнения локализации и определения степени аортального стеноза.
Клинические проявления
В отличие от других пороков сердца, выраженный стеноз аорты может длительное время протекать без клинических проявлений. Дети растут и развиваются нормально.
При наличии жалоб больные отмечают утомляемость, одышку при нагрузке, боли за грудиной и головокружение. Реже жалуются на боль в животе, профузную потливость, носовые кровотечения. Быстрая утомляемость и одышка при нагрузке свидетельствуют о сужении средней тяжести.
Головокружение при нагрузке является признаком резкого сужения аорты и объясняется неспособностью левого желудочка увеличить выброс, чтобы поддержать адекватный церебральный кровоток. Ангинозные боли возникают из-за несоответствия доставки кислорода в левый желудочек потребностям миокарда.
Если стеноз аорты проявляется выраженной симптоматикой в период новорожденности, он определяется как «критический», ассоциируется с непосредственной угрозой для жизни и необходимостью неотложного вмешательства. В большинстве случаев имеется двустворчатый аортальный клапан.
Аускультация. На верхушке сердца слышен аортальный тон выброса, если клапан подвижный. Тон генерируется открывающимися створками, его интенсивность не изменяется во время дыхания. Наличие IV сердечного тона указывает на тяжелую обструкцию, поскольку гипертрофия препятствует пассивному наполнению левого желудочка. Также выслушивается громкий, грубый и систолический шум стеноза аорты, лучше слышен у основания сердца.
Лечение
Деформированный аортальный клапан является потенциальным местом бактериальной инфекции, поэтому необходимо уделять постоянное внимание профилактике инфекции вне зависимости от тяжести сужения.
Методы хирургического лечения адаптированы к состоянию больных, возрасту и форме порока.
- У младенцев, находящихся в тяжелом состоянии, методом выбора является чрескожная баллонная вальвулопластика.
- У старших детей выполняют аортальную вальвулотомию на открытом сердце.
- Протезирование аортального клапана может оказаться неизбежным при одностворчатом или дисплазированном двустворчатом клапане, а также у старших детей и взрослых после предшествующей вальвулотомии в связи с прогрессирующими дегенеративными изменениями и кальцификацией.
- Аутотрансплантация собственного легочного ствола с клапаном в аортальную позицию и восстановлением выводного тракта правого желудочка гомографтом (операция Rоss).
- Больные с тяжелым сужением клапанного кольца или туннелевидной обструкцией нуждаются в расширении корня аорты (операция Konno) в сочетании с протезированием клапана или операцией Ross (Ross–Konno).
Субаортальный стеноз
Анатомия
Субаортальный стеноз - подклапанное сужение выводного отдела левого желудочка, чаще всего в виде мембраны или фиброзного кольца. Существует несколько анатомических вариантов порока: дискретная мембрана, структурный субаортальный стеноз и туннельная форма. Дискретная субаортальная мембрана - сужение компонента ВОЛЖ за счет фиброзной мембраны с центрально расположенным отверстием.
Структурный субаортальный стеноз - циркулярное фиброзное утолщение в виде валиков. При туннельной форме существует фиброзно-мышечная складка, охватывающая ВОЛЖ по типу воротника. Обструктивная ГКМП также относится к группе пороков с субаортальным стенозом.
Гемодинамика
Нарушения гемодинамики характеризуются наличием препятствия на пути системного оттока. Градиент систолического давления при данном пороке возникает внутри самого желудочка, основным механизмом компенсации является повышение давления в левом желудочке. В последующем развивается гипертрофия миокарда, увеличение давления в левом предсердии, что в конечном итоге приводит к левожелудочковой сердечной недостаточности.
Диагностика
- ЭхоКГ, КТ, МРТ. Визуализация дефекта.
- Рентгенография органов грудной клетки. При выраженном стенозе на рентгенограмме наблюдается расширение контура левого желудочка и сердце имеет аортальную конфигурацию с резко выраженной «талией».
- ЭКГ. Признаки гипертрофии левого желудочка.
Клинические проявления
У новорожденных и детей раннего возраста субаортальный стеноз в изолированном виде практически не встречается и проявляется только в возрасте после года жизни. В раннем возрасте в большинстве случаев он встречается как сопутствующая патология и клиника заболевания «маскируется» основным пороком. У более взрослых детей (после 3 лет) и у некоторых взрослых даже выраженный стеноз может протекать бессимптомно. Основными жалобами больных являются: одышка, повышенная утомляемость, боли в области сердца. Одна из клинических особенностей порока — обморочные состояния.
Усиленный приподнимающийся верхушечный толчок, несоответствие между ним и редким малым пульсом. У всех больных выслушивается звучный систолический шум над основанием сердца или в III межреберье слева с иррадиацией на шею и в яремную ямку. Характерно систолическое дрожание над сонными артериями.
Лечение
Для лечения данного порока применяется хирургическое лечение. Применяются операция Конно и ее модификации, резекция подклапанного стеноза аортального клапана. Также часто применяется эндоваскулярные методики: транслюминальная баллонная дилатация.
Надклапанный аортальный стеноз
Анатомия
Надклапанный стеноз аорты - диффузное или локальное сужение восходящей аорты выше синотубулярной зоны. Морфологически - фиброз и разрастание эндотелия. По форме стеноза он может быть: в виде мембраны, локального сужения (по типу песочных часов) или диффузный стеноз.
Гемодинамика
Аналогично другим обструкциям выводного отдела левого желудочка гемодинамически это характеризуется гипертрофией и перегрузкой левого желудочка и, в последующем, развитием левожелудочковой сердечной недостаточности. Также важным признаком является расположение коронарных артерий проксимальней места стеноза и подвергаются постоянному воздействию высокого давления.
Диагностика
- ЭхоКГ, КТ, МРТ. Визуализация дефекта.
- ЭКГ. Признаки гипертрофии левого желудочка.
Клинические проявления
Признаки надклапанного стеноза аналогичны симптомам, присущим другим типам аортальных стенозов, хотя ангинозные боли отмечаются чаще.
Несмотря на то что аускультативные данные при всех типах аортального стеноза схожи, при надклапанном типе отсутствует систолический щелчок над аортальным клапаном и эпицентр систолического шума расположен выше, чем при субаортальном стенозе. Тон закрытия аортального клапана акцентуирован вследствие повышения давления в аорте проксимальнее места сужения.
Артериальное давление на правой руке может быть выше, чем на левой, что, возможно обусловлено сужением дуги аорты или подключичной артерии. Пульс на левой руке также может быть ослаблен.
Лечение
По мере роста ребенка происходит прогрессирование изменений со стороны аорты, развивается характерная клиническая картина порока и возникает необходимость его хирургической коррекции, обычно в возрасте от 2 до 20–30 лет. Показаниями к оперативному лечению являются: наличие клинической симптоматики, градиент давления в области стеноза более 50 мм рт. ст. и нарушение коронарного кровообращения.
Для хирургической коррекции применяются методики пластического расширения восходящей аорты.