Коарктация аорты
Что такое Коарктация аорты?
Коарктация аорты – врожденный порок сердца, характеризующийся наличием сегментарного сужения аорты, которое может локализоваться на любом ее участке.
Эмбриология
У нормального эмбриона область перешейка аорты бывает сужена, т.к. во внутриутробный период только третья часть кровотока проходит через него в нисходящую аорту. Остальная часть кровотока попадает в нисходящую аорту через артериальный проток из легочной артерии. При наличии сопутствующих пороков сердца, которые создают дисбаланс между выводными трактами правого и левого желудочков, возникает еще большая зависимость развития перешейка аорты от функции артериального протока. Увеличение функции протока приводит к патологическому сужению перешейка.
Считается также, что коарктация аорты является следствием патологического кровообращения плода в случаях, когда имеется препятствие выбросу в восходящую аорту.
При наличии стенозирующего двустворчатого аортального клапана увеличивается поток крови справа налево через ОАП в период внутриутробного развития, что способствует миграции тканей протока в прилежащую стенку аорты.
Ткани протока вместе с гладкомышечными клетками распространяются по всему периметру аорты. Дуктальные ткани со временем фиброзируются, что приводит к сужению данного сегмента аорты.
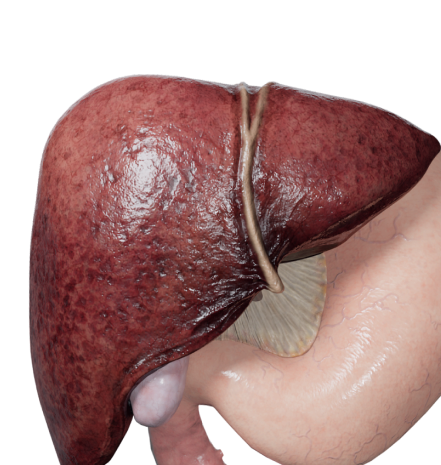
Анатомия
Морфологически в зоне коарктации обнаруживается скопление гладкомышечных клеток и миксоматозной ткани. Существует теория о том, что данные клетки мигрируют в зону аорты из артериального протока. Наиболее частое расположение коарктации - зона нисходящей аорты после отхождения левой подключичной артерии. Редко сегментарное сужение аорты может встречаться в любой ее части. Существует 3 анатомических типа коарктации аорты: преддуктальный (детский тип), постдуктальный (взрослый тип) и юкстадуктальный.
Юкстадуктальный тип (неонатальный) - зона коарктации находится на уровне артериального протока, закрытие которого приводит к быстрому развитию сердечной недостаточности, т.к. вместе с артериальным протоком сужается и зона коарктации. Помимо сужения аорты при изолированной коарктации можно обнаружить гипертрофию и нарушение сократимости левого желудочка. Частыми сопутствующими аномалиями являются: гипоплазия дуги аорты, бикуспидальный аортальный клапан, СГЛОС, ЕЖС с обструкцией системного кровотока и другие.
Классификация
- Предуктальная;
- Юкстадуктальная;
- Постдуктальная.
Гемодинамика
При наличии критической неонатальной коарктации во внутриутробном периоде, кровоснабжение нижней части тела осуществляется через артериальный проток, что поддерживается высоким легочным сопротивлением.
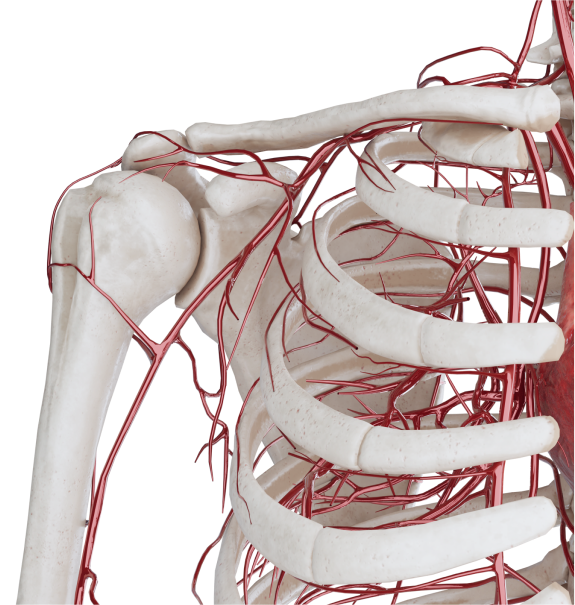
При закрытии протока после рождения, происходит быстрое развитие сердечной недостаточности. Клинически проявляется отсутствием пульсации на бедренных артериях, ребенок становится вялым. Одновременно с этим увеличивается легочной кровоток, что приводит к развитию отека легких. Со временем прогрессирует ацидоз, развивается полиорганная недостаточность, что в конечном итоге приводит к смерти. При медленном закрытии преддуктальной коарктации гемодинамические нарушения заключаются в уменьшении перфузии нижней части тела, резкого развития тяжелых органных нарушений, как правило, не происходит. При взрослом типе коарктации аорты формируются коллатеральные сосуды, через которые происходит кровоснабжение нисходящей аорты. При таком типе порока часто диагноз не устанавливается вовремя, клинически можно наблюдать разницу давления на руках и ногах и незначительное отставание в физическом развитии.
Диагностика
- ЭхоКГ, КТ, МРТ. Визуализация дефекта и сопутствующих пороков.
- ЭКГ. В первые месяцы жизни преобладают признаки нагрузки на правые отделы сердца. С 6-12 месяцев преобладают признаки перегрузки левых отделов сердца.
- Рентгенография органов грудной клетки. Умеренный венозный застой в легких, увеличение размером сердца.
- Катетеризация сердца и ангиокардиография. Применяют в случаях, когда не ясен характер сопутствующих ВПС или есть подозрение на перерыв дуги аорты.
Клинические проявления
Клиническая картина коарктации аорты зависит от возраста пациента, наличия сопутствующих аномалий сердца и анатомических особенностей порока. У многих детей с данным пороком сердца наблюдается непропорциональное развитие тела: нижняя половина тела меньше верхней. В некоторых случаях, можно определить сильную пульсацию сонных и подключичных артерий, разницу артериального давления на нижних и верхних конечностях.
Для детей с преддуктальной коарктацией и открытым артериальным протоком характерен дифференциальный цианоз: верхняя часть тела нормального цвета, нижние конечности цианотичные. На лучевых артериях определяется сильный, хорошего наполнения пульс. При пальпации верхних отделов грудной клетки выявляют пульсацию коллатеральных сосудов. Пульсация брюшной аорты и бедренных артерий значительно ослаблена или отсутствует. Артериальное давление повышено на верхних конечностях, наличие градиента давления между верхними и нижними конечностями.
Сердечный толчок у пациентов может быть усилен. Во ІІ–ІІІ межреберных промежутках слева выслушивается интенсивный систолический шум. Он распространяется на сосуды шеи и в межлопаточное пространство, больше с левой стороны. Шум создается струей крови, проходящей через сужение и коллатеральные сосуды, и колебаниями аортальной стенки.
Особое внимание необходимо уделять функции ОАП у новорожденных с преддуктальной коарктацией, так как закрытие протока у таких детей приводит к острой гипоперфузии нижней половины туловища, развитию сердечной недостаточности, нарушению функции почек.
Лечение
Консервативная терапия направлена на снижение метаболических потребностей организма, лечение сердечной недостаточности, симптоматическую терапию.
Отсутствие эффекта от консервативной терапии, большая вероятность тяжелых осложнений некорригированного порока, хорошие непосредственные и отдаленные результаты устранения коарктации аорты сделали хирургический метод лечения общепризнанным. По поводу «хирургического возраста» пациентов большинство авторов сходятся во мнении, отдавая предпочтение раннему вмешательству.
Чаще используют несколько принципиально отличных типов операции, а именно: резекцию сужения с анастомозом «конец в конец», расширенный анастомоз при наличии сопутствующей гипоплазии дуги аорты, варианты пластики с использованием подключичной артерии и, в редких случаях, расширение с помощью заплаты или протезирование. Для уменьшения риска рекоарктации аорты необходимо полностью иссекать зону сужения, т.к. находящаяся в ней миксоматозная ткань будет приводить к развитию коарктации в отдаленном периоде.
Также применяются эндоваскулярные методы коррекции: баллонная дилятация и стентирование. Рентгеноэндоваскулярная баллонная дилатация чаще используется для повторной коарктации. Первичное ее применение ограничено из-за высокой частоты рекоарктаций. Стентирование зоны коарктации также используется редко.
При наличии сопутствующих аномалий сердца часто возникают приступы сердечной декомпенсации в большом круге кровообращения (периферические отеки, гепатомегалия) или в малом круге (отек легких, цианоз). В таких случаях коррекцию необходимо выполнять по жизненным показаниям.